


Nascent motor unit potentials that have a prolonged duration and asynchronous waveforms may appear weeks to months later if there is reinnervation. The EMG may show evidence of membrane instability, as manifested by increased insertional activity, fibrillation potentials, and positive sharp waves and axonotmesis and neurotmesis after 3 weeks. In a neurapraxic lesion, the distal conduction velocity is normal and the EMG will be normal. A nerve conduction study may reveal a complete conduction block across the injury site, but this will also be present in both axonotmesis and neurotmesis. With damage to the PIN, wrist, finger, and thumb extension is absent.Įlectrodiagnostic testing is usually done after 3 to 4 weeks from the time of injury to allow time for fibrillation potentials to occur. A PIN injury results in sparing of the ECRL and ECRB function, but there is paralysis of the ECU, which results in radial wrist deviation during attempted extension. Radial nerve injury at the distal arm will spare the brachioradialis, which is tested by asking the patient to flex the forearm with the forearm in neutral rotation.Īn elbow-level radial nerve injury causes loss of function of the ECRL and ECRB muscles. Injury to the radial nerve at a midarm level secondary to a humeral fracture may present with paralysis of the brachioradialis and forearm at wrist extensors with sparing of the triceps. If the patient is seated, the patient is asked to extend the elbow so that the forearm is parallel to the floor.

The triceps is tested with the shoulder partially abducted and the elbow partially flexed to avoid the effects of gravity. If a patient presents with an isolated deltoid and triceps palsy in the presence of normal wrist extension, the site of injury is the axilla at the point where the axillary nerve and the main nerve supply to triceps are closely related to one another. Radial nerve injuries usually lead to a complete deficit rather than partial deficit.Ī neurological assessment should be performed before and after either open or closed manipulation of a humeral fracture to evaluate for a worsening neurological deficit.
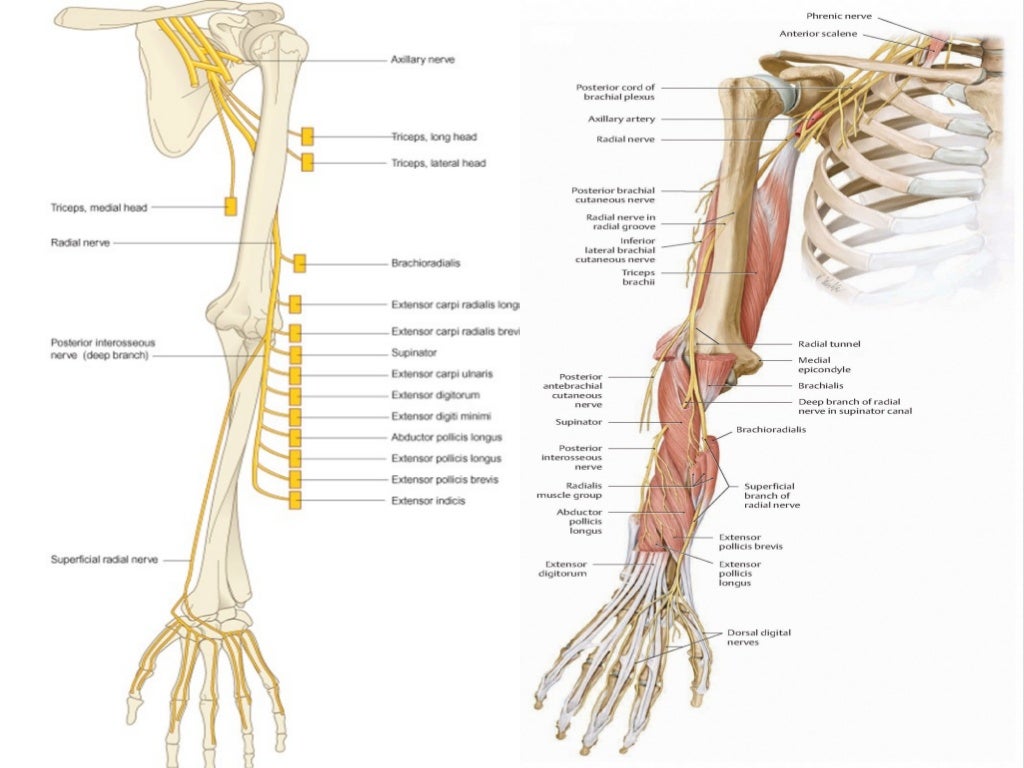
Nerve injuries associated with fractures and dislocations are classified according to Seddon′s classification (neurapraxia, axonotmesis, and neurotmesis). The radial nerve is injured in 10 to 20% of humeral fractures, and the nerve injury usually occurs at the time of the fracture rather than as a consequence of manipulation. The sensory deficit from an injury to the superficial radial nerve branch includes the radial aspect of the distal forearm and the first web space, but this is variable. The hallmark of a radial nerve injury in the axilla is triceps weakness, whereas injuries at the distal humerus spare the triceps and lead to weakness of the wrist and forearm extensor muscles, as well as the brachioradialis. In the forearm, muscles that are supplied by one of the radial nerve′s terminal branches, the posterior interosseus nerve (PIN), include the supinator, the extensor carpi ulnaris (ECU), the ECRL, the extensor digitorum communis (EDC), the extensor indicis (EIP), the extensor digiti minimi (EDM), the extensor pollicis brevis (EPB), the extensor pollicis longus (EPL), and the abductor pollicis longus (APL). The radial nerve innervates the triceps, anconeus, brachioradialis, extensor carpi radialis longus (ECRL), and extensor carpi radialis brevis (ECRB) muscles. Radial Nerve Repair/Graft Terrie Koo, Suparna Saha, Sangkook Lee, and Daniel H.


 0 kommentar(er)
0 kommentar(er)
